Understanding Dual Diagnosis
- Oct 5, 2022
- 11 min read
Updated: Oct 20, 2025

Addressing underlying mental health issues is critical for successful substance abuse treatment. Without tackling co-occurring disorders like depression, anxiety, and PTSD, the likelihood of a successful recovery diminishes significantly. We'll explore why a comprehensive approach is the most effective way to achieve lasting wellness.
What is the most effective approach for treating dual diagnosis?
The most effective approach for treating dual diagnosis is integrated treatment. This method coordinates substance use and mental health care simultaneously, addressing both issues at once to prevent relapse and support a more complete recovery.
If you're seeking a deeper understanding of dual diagnosis, co-occurring disorders, and the specific treatments available, you've come to the right place. We'll break down the differences between these conditions, identify key symptoms, and discuss the various therapeutic approaches that lead to a healthier, transformed lifestyle.
The Importance of Addressing Underlying Mental Health
It is important to treat Dual Diagnosis because studies have shown that without addressing the underlying mental health issues, there is a less likelihood for success when treating substance abuse. Dual diagnosis patients often suffer from depression, anxiety, PTSD, and trauma; these conditions are commonly treated with medication or therapy in order to help manage symptoms.
Dual Diagnosis treatment centers focus on both substance abuse and mental health issues, which makes them an ideal choice for Dual Diagnosis patients. Dual Diagnosis treatment is also more effective because it addresses the root cause of addiction rather than just treating symptoms.
Dual diagnosis patients are more likely to recover successfully when they receive dual diagnosis care at a specialized center instead of traditional rehab. Dual diagnosis patients also benefit from treatment programs that address both substance abuse and mental health issues at once rather than treating them separately, which can be confusing for some patients who suffer from multiple conditions simultaneously.
The most common combinations are:
Dual diagnosis of depression and alcohol use disorder
Dual diagnosis of anxiety and cocaine use disorder
Dual diagnosis of bipolar disorder and methamphetamine addiction
Jump to Section:

Suffering from addiction or a mental health disorder is a very complicated and nuanced ordeal. A number of personalized coping strategies are needed for each individual’s unique situation. Dual Diagnosis can further complicate one’s circumstances. It can prompt the need to further personalize and address one’s specific symptoms, mindset, and the interplay between addiction and mental health disorders.
However, despite being a complicated situation, a dual diagnosis can still be effectively addressed and overcome. It is necessary to take a personalized approach to best understand one’s unique diagnoses, needs, and hurdles when creating a plan for a healthier and transformed lifestyle.
What Is Dual Diagnosis?
Dual Diagnosis is a comprehensive holistic mental health and substance use treatment method. Many times, individuals seeking treatment for substance use disorders – a mental disorder that, according to the National Institute of Mental Health (NIMH), “affects a person’s brain and behavior, leading to a person's inability to control their use of substances” – also suffer from mental health issues. These are called co-occurring mental disorders.
About 50% of people suffering from SUD will experience a co-occurring mental disorder, which can include anxiety disorders, depression, and personality disorders.
SUDs do not always lead to co-occurring mental disorders, but it does happen. Sometimes mental illness is caused by substance use. Other times, you may turn to substance use to cope with your anxiety or depression. Regardless of which began first, both kinds of disorders exacerbate each other. You cannot truly treat one by treating the other.
If you are seeking treatment for SUD, you must address your co-occurring mental disorders as well. If you do not, you will be at a greater risk of experiencing relapse early on in recovery. It will be more difficult if you have both a mental illness and addiction to recover. When seeking treatment, you should be mindful to consider if facilities are capable of treating co-occurring mental disorders.
What Are Co-Occurring Disorders?
Co-occurring disorders, or co-diagnosis, are a more specific subcategory of dual diagnosis that refers to an individual who suffers from a substance use disorder or addiction and a mental health disorder.
For some, this can mean they have developed a mental health disorder due to their use of drugs, alcohol, or other addictive substances or practices. However, others will develop co-occurring disorders as they attempt to self-medicate their anxieties, depression, bipolar disorder, or other mental health concerns with addictive substances.
Regardless of if mental health begets the use of addictive substances or the other way around, co-occurring disorders require an individual to address both their mental health and self-medication practices simultaneously to move towards a sustained healing practice.
The Difference Between Dual Diagnosis and Co-Occuring Disorders
The biggest difference between co-occurring disorders and dual diagnosis comes down to the nature of the diagnosis. Co-occurring disorders are specifically tied to the use of an addictive substance, such as cocaine, heroin, alcohol, or methamphetamines, and the effect that these substances have on one’s mental health.
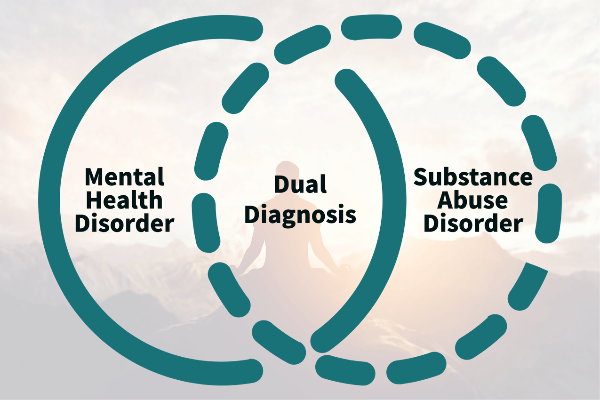
However, dual diagnosis can be used to refer to any two diseases afflicting a person in tandem, regardless of their nature.
While all co-occurring disorders can also be referred to as dual diagnoses, not all dual diagnoses will necessarily be classified as co-occurring disorders, even if the two terms are often used interchangeably.
What Does Dual Diagnosis Treatment Look Like?
Dual diagnosis requires the diagnosis of co-occurring disorders first. Co-occurring disorders – according to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) – must include a combination of at least one SUD and one mental disorder.
These combinations can look different for everyone. Common mental disorders you might typically face are anxiety and mood disorders, schizophrenia, bipolar disorder, post-traumatic stress disorder (PTSD), and attention deficit hyperactivity disorder (ADHD). The most common substances that are abused include alcohol, tobacco, opioids, stimulants, hallucinogens, and prescription drugs.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), integrated treatment coordinates substance use and mental health treatment. These integrated treatments are the best course of action for treating addiction and co-occurring disorders. Of course, integrated treatment should be individualized to your needs. Only then will it be most effective.
Thankfully, more treatment facilities have begun implementing integrated treatment into their programs over the years. Integrated treatment typically includes behavioral therapies like:
Cognitive-behavioral therapy (CBT)
Cognitive Behavioral Therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders.
CBT focuses on challenging and changing cognitive distortions (such as thoughts, beliefs, and attitudes) and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems.
Psychotherapy
Psychotherapy is also known as talk therapy. and is type of mental health treatment.
It’s often used either alone or with medications to treat mental disorders. During a psychotherapy session, you talk to a doctor or a licensed mental health care professional to identify and change troubling thoughts.
Benefits include:
Understanding behaviors, emotions, and ideas that contribute to the illness
Understanding and identifying life problems or events
Regaining a sense of control in life
Learning healthy coping techniques and problem-solving skills
Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) is the use of medications, in combination with counseling and behavioral therapies, to provide a “whole-patient” approach to the treatment of substance use disorders.
Research shows that a combination of medication and therapy can successfully treat these disorders, and for some people struggling with addiction, MAT can help sustain recovery. MAT is also used to prevent or reduce opioid overdose.
Dialectical behavior therapy (DBT)
An evidence-based psychotherapy that began with efforts to treat personality disorders and interpersonal conflicts. Evidence suggests that DBT can be useful in treating mood disorders and suicidal ideation, as well as for changing behavioral patterns such as self-harm and substance use. DBT evolved into a process in which the therapist and client work with acceptance and change-oriented strategies, and ultimately balance and synthesize them
Assertive Community Treatment (ACT)
A type of community-based mental health care. It emphasizes providing locally-based treatment for you if you are struggling with addiction and co-occurring mental disorders.
Medication
Some medications may be prescribed to dual diagnosis patients in order to help manage their mental health symptoms. Medication for dual diagnosis disorders helps to decrease symptoms and stabilize the addict’s mood.
Most mental health medications (such as Antidepressants, Antipsychotics, Anticonvulsants, Beta Blockers, Sedative/Hypnotics, and Sleep Aids) will take 4-6 weeks to be fully active within the addict’s bodySome medications may be prescribed to dual diagnosis patients in order to help manage their mental health symptoms. Medication for dual diagnosis disorders helps to decrease symptoms and stabilize the addict’s mood.
Most mental health medications (such as Antidepressants, Antipsychotics, Anticonvulsants, Beta Blockers, Sedative/Hypnotics, and Sleep Aids) will take 4-6 weeks to be fully active within the addict’s body
Specialized Treatment Centers
There are many specialized treatment centers that offer comprehensive care for dual diagnosis patients. According to the National Institute of Mental Health (NIMH), approximately half of all people with a substance use disorder of addiction will also experience some form of mental health disorder in their lifetime.
Expert Dual diagnosis treatment is necessary to diagnose and treat both addiction and mental illness together by isolating the root causes of each condition and finding the most appropriate ways of healing each of them simultaneously.
These are just few out of an array of evidence-based therapies that may be utilized in dual diagnosis. It can take some time to find the right combination of treatments. The NIMH also discusses the effectiveness of medications for treating addiction and co-occurring mental disorders.
Medications are sometimes used to help with the symptoms of withdrawal that many experiences during detox. By not seeking treatment, you risk falling into a vicious cycle of suffering between both disorders. Regardless of which came first, mental illness or addiction, both will wreak havoc in endless ways.
Identifying Various Symptoms
Dual diagnosis is a very personal combination of unique symptoms, making it can be difficult to determine specific symptoms that apply to all circumstances. However, being vigilant to identify overall changes can indicate there is a need to seek professional help, or that an individual may be coping with multiple stressors simultaneously. Some things to look for include:
Sudden changes in social outings, resulting in isolation or disinterest in previous hobby groups
Difficulty maintaining employment or inconsistent attendance at work
Pervasive and consistent feelings of worry, panic, or confusion
An increase in risky behaviors
Sudden changes in overall mood
Inability to maintain daily responsibilities
Compromised hygiene routine or eating schedule
Difficulty maintaining meaningful relationships
These are only a few ways in which an individual may present multiple complications at once. An individual’s unique combination of diagnoses can make it difficult to determine how many diagnoses they may be suffering from without the trained eye of a professional to guide them. Educating oneself about a loved one’s diagnosis can help determine if their symptoms are the result of a diagnosis, or if there may be additional hurdles in their recovery.
The Cyclic Nature of Dual Diagnosis
Suffering from a dual diagnosis of any kind can create a complicated recovery path. However, recovery is always possible, even if an individual may need to plan their recovery journey in a unique way. Those suffering from a dual diagnosis will need to address their recovery on all fronts in order to create the best approach to a sustained and effective recovery.
Those suffering from dual diagnosis may find that their substance abuse disorders and mental health disorders can continue to impact each other. For example, one’s anxiety disorder can make it very difficult to manage their coping strategies when dealing with urges to reengage with cocaine. This may make it easier to begin using the addictive substance again. Likewise, one’s use of a drug can also increase one’s debilitating feelings of anxiety.
Addressing one’s use of drugs without addressing one’s anxiety disorder can lead to a very difficult and fragile recovery if there are no strategies in place to quell feelings of anxiety. This can increase the chances of relapse, just as addressing one’s anxiety without confronting the role that drug use has played can make many coping strategies difficult to employ. Anxiety then may continue to affect one’s life.
Honesty is Key

One of the most important factors in dual diagnosis therapy is getting honest. This means being truthful with your therapist and family members about your addiction and mental health condition. It can be one of the most difficult things to do, but it’s a critical step in treatment. If you’re not honest, then you won’t be able to get the most out of therapy.
You also won’t be able to build trust with your therapist or family members. This can make it difficult to get the support you need during treatment. Being honest is also important because it allows you to understand your addiction and mental health condition better. When you know what’s going on then you can start making the changes needed to overcome it.
For example, if someone is addicted to opioids, but they don’t know it and aren’t honest about their use of them, they won’t be able to begin treatment. They also won’t be able to overcome their addiction if they don’t know what it is. It can also be difficult for people to get honest about their mental health condition, because of the stigma surrounding these conditions. But being honest allows you to start working on your therapy and recovering from your dual diagnosis.
Getting honest can be difficult, but it’s an important step in the dual diagnosis therapy process. You need to be able to trust your therapist and family members during treatment. This will help you get the support you need. And being honest about your addiction and mental health condition is also necessary for getting better.

Treatment at Chateau Recovery's Utah Facility
Chateau Recovery offers treatment in order to help you seek treatment and improve your life. Recovery is something you have to want for yourself. If you decide you want to change your life, Chateau offers a safe and peaceful setting to do so. Our luxurious feeling facility, based amidst the natural beauty of Utah, is a perfect spot to focus on your path to recovery. You will experience individual attention and treatment, an intimate group setting, and access to resources during and after your stay.
Your path to recovery does not stop when you leave Chateau Recovery. Our alumni network can be an excellent tool in aiding you on your path to recovery upon leaving the facility. The path to recovery does not end. Addiction and mental illness are chronic disorders that you must face throughout your life. Staying connected with the people you meet during your time here makes that burden a little less heavy.
In addition to staying connected to other alumni, Chateau will do the same. We believe in staying in touch with you for continued support. Whether you are struggling to integrate back into your everyday life, or are finding difficulty in the challenges of early recovery, we want to continue being there for you. You have to first want a life of recovery for yourself.
If you or someone you love is exhibiting signs of mental illness, addiction, or both, reach out to Chateau Recovery today. Together we can determine if dual diagnosis at our Utah facility is the right fit for you, and if so, how we can get you set on your path to recovery today.
Frequently Ask Questions:
• What is dual diagnosis?
Dual diagnosis is a treatment method that addresses both a substance use disorder and a co-occurring mental health issue. It is a holistic approach to care.
• What are some common combinations of dual diagnosis?
Common combinations include depression and alcohol use disorder, anxiety and cocaine use disorder, and bipolar disorder and methamphetamine addiction.
• What is the difference between dual diagnosis and co-occurring disorders?
While the terms are often used interchangeably, co-occurring disorders specifically refer to a substance use disorder combined with a mental health disorder. Dual diagnosis can refer to any two diseases afflicting a person in tandem.
• What types of therapies are used in dual diagnosis treatment?
Integrated treatment for dual diagnosis often includes behavioral therapies such as Cognitive-Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), Psychotherapy, and Medication-Assisted Treatment (MAT).
• Why is honesty important in dual diagnosis treatment?
Honesty is crucial because it allows the patient to build trust with their therapist and family, get the most out of treatment, and better understand their conditions to make the necessary changes for recovery.
When you're ready to take the next step on your path to recovery, we're here to help. Our team at Chateau Health and Wellness Treatment Center understands the complexities of dual diagnosis and is committed to providing the personalized, integrated care you deserve. We've built our program on a foundation of empathy and expertise, creating a safe and peaceful environment where you can focus on healing. If you or a loved one is struggling with addiction and a co-occurring mental health disorder, give us a call at (435) 222-5225. Together, we can create a plan to help you reclaim your life and build a healthier, more fulfilling future.

About The Author
Ben Pearson, LCSW - Clinical Director
With 19 years of experience, Ben Pearson specializes in adolescent and family therapy, de-escalation, and high-risk interventions. As a former Clinical Director of an intensive outpatient program, he played a key role in clinical interventions and group therapy. With 15+ years in wilderness treatment and over a decade as a clinician, Ben has helped countless individuals and families navigate mental health and recovery challenges.








