

UNDERSTANDING THE WHOLE SELF
What is Dual Diagnosis?
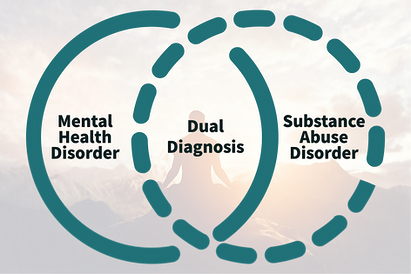
Defining Dual Diagnosis
Dual Diagnosis treatment is an approach where the person struggles with both substance use disorders and mental health issues. Dual diagnose therapies are designed so individuals receive support specifically tailored towards treating co-occurring conditions simultaneously rather than having to cycle through treatments separately.
If a person has both mental illness and addiction, it is more difficult for them to recover. Rehabilitation will be less effective if not treated properly because the two conditions interact in negative ways which makes rehabilitation complex and risky overall.
Dual Diagnosis Origins
The term dual diagnosis emerged in the 1980s to describe individuals dealing with both mental health and substance use disorders. Previously treated separately, it became clear that integrated care was needed for effective recovery, leading to specialized approaches that address both conditions together.
Diagnosing Co-occuring Disorders
Co-occurring disorders include a combination of two or more substance use disorders and mental disorders as identified in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
There are no specific combinations of mental and substance use disorders that are defined uniquely as co-occurring.
Why Do Substance Abuse Disorders and Mental Health Disorders Occur Together?
Although these problems often occur together, this does not mean that one caused the other, even if one appeared first. In fact, it can be hard to figure out which came first. Researchers think that there are three possibilities as to why they occur together:
-
Common risk factors may contribute to both mental disorders and substance use disorders. These factors include genetics, stress, and trauma.
-
Mental disorders can contribute to drug use and substance use disorders. For example, people with mental disorders may use drugs or alcohol to try to feel better temporarily. This is known as self-medication. Also, mental disorders may change the brain to make it more likely you will become addicted.
-
Substance use and addiction can contribute to the development of a mental disorder. Substance use may change the brain in ways that make you more likely to develop a mental disorder.


UNDERSTANDING
Causes of Dual Diagnosis
Mental health disorders are more likely to lead someone into substance abuse. The National Institute on Drug Abuse reports that half of all individuals who have either a mental illness or abuse a substance will go onto develop another problem at some point during their lives, usually as part of an overlapping cycle.
Symptoms of Dual Diagnosis
The symptoms of co-occurring disorders can be overwhelming. Coexisting conditions affect an individual's mental health and substance use problem in addition to their day to day, including:
-
Symptomatic relapses
-
Hospitalizations
-
Financial challenges
-
Social isolation or avoidance
-
Physical and/or sexual victimization
-
Serious medical illness
Mental health conditions that commonly co-occur with substance use disorders include anxiety disorders, depressive disorders, ADHD, bipolar disorder, schizophrenia, and personality disorders, according to the National Institute of Mental Health.
Which Develops First: Mental Illness or Addiction?
Many times, and this may be the most common scenario with co-occurring disorders, someone with a mental illness will self-medicate with drugs and/or alcohol as a way to deal with their depression, trauma, or anxiety disorder.
Chronic substance use can lead to various other disorders such as depression, mood or eating problems. It’s important for that person's mental health and they need treatment in order not only prevent further illness but also achieve long-term sobriety.
Regardless of the path a person takes to the co-occurring disorder, there’s there’s always a path forward to long-term sobriety and mental health.

UNDERSTANDING
Important Notes
It's Not Uncommon to Receive Dual Diagnosis
Dual diagnosis is an unfortunate reality for many people. It can happen to anyone, regardless of their mental illness or addiction alone- the two are often paired together.
There Are Many Versions of Dual Diagnosis
Dual diagnosis patients have one or more mental disorders (including anxiety disorder, depression, etc.) and addictions (alcohol, drugs, gambling, etc.).
Many diagnoses get initially made based on visible symptoms more commonly seen in addiction but dual diagnosis treats the symptoms and the underlying causes.
Those with Mental Illnesses Are More Prone to Addiction
According to the DSM-5, an increased risk of alcohol use disorder, for example, is associated with conditions including bipolar disorders, schizophrenia, and antisocial personality disorder.
Other substance-related disorders also commonly co-occur with distinct psychiatric conditions. As in the case of opioid use and depressive disorders, it is possible that a substance use problem leads to the development of other mental health challenges or a worsening of any preexisting disorders.
-
Roughly 50% of individuals with severe mental disorders are affected by some form of substance abuse or dependence.
-
37% of people who are dependent upon or abuse alcohol and 53% of people who are dependent upon or abuse street drugs also have at least one serious mental illness.
According to a report in the Journal of the American Medical Association (JAMA)


TREATMENT
Approach to Treatment
The Substance Abuse and Mental Health Services Administration (SAMHSA) stresses that integrated treatment is the best course of action for co-occurring disorders. Integrated approaches coordinate substance abuse and mental health treatments, rather than treating each separately.
A program that treats co-occurring disorders may include psychoeducational classes and relapse prevention education. These help individuals with mental illness, as well as those who abuse substances understand the symptoms of their condition better so they know when it is appropriate for them to seek medical attention
Screening Is Standard Now
Addiction treatment centers now screen for mental illness during the admission process as part of their standard operating procedures. To screen people for depression, for example, we use the PHQ-9 test protocol. For anxiety disorder, it’s the GAD-7 test.
Tailored Treatment for Co-occurring Disorders
As for the treatment that then needs to happen, many addiction treatment centers have specialists whose training is in various mental illnesses and the entire staff often receives supplemental training in mental illness so they can recognize symptoms, tailor treatment programs, and handle integrated treatment requirements.

TREATMENT
Integrated Treatment
Mental illnesses and substance use disorders have been historically treated as two separate issues. However, there is now an increase in integrated treatment centers that address both problems from the beginning of one’s recovery process and/or immediately following detox/stabilization. Addiction specialists are trained how to screen for mental health conditions while therapists are knowledgeable about asking patients about substance use.
Integrated treatment often involves Behavioral treatment often includes forms like cognitive-behavioral therapy and dialectical behavior modification that can help improve coping skills, reduce maladaptive behaviors and can be used in combination with medication.
Why is Integrated Treatment Important
Integrated treatment is key because it treats all conditions holistically rather than in isolation. For example, studies have found, for example, that depression quadruples the risk of relapse in alcoholics in the first year of recovery. Addressing mental health conditions and other underlying issues is key for long-term sobriety and health.

Dual Diagnosis Benefits




Comprehensive Treatment
Addresses both mental health and substance use disorders simultaneously for lasting recovery.
Improved Outcomes
Reduces relapse risk by treating the root causes of addiction and mental health struggles.
Personalized
Care
Tailors treatment to individual needs, ensuring a more effective recovery process.
Stronger Support Network
Provides integrated therapy and community resources for long-term stability.

HOW WE HELP
Using Dual Diagnosis at Chateau
At Chateau, we specialize in dual diagnosis treatment, addressing both mental health and substance use disorders together for a comprehensive recovery approach. Our expert clinicians provide personalized care, using evidence-based therapies tailored to each client’s needs.
With a 1:4 clinician-to-client ratio, a trauma-informed team, and a serene, private setting, we ensure the support and resources necessary for long-term healing and stability.

